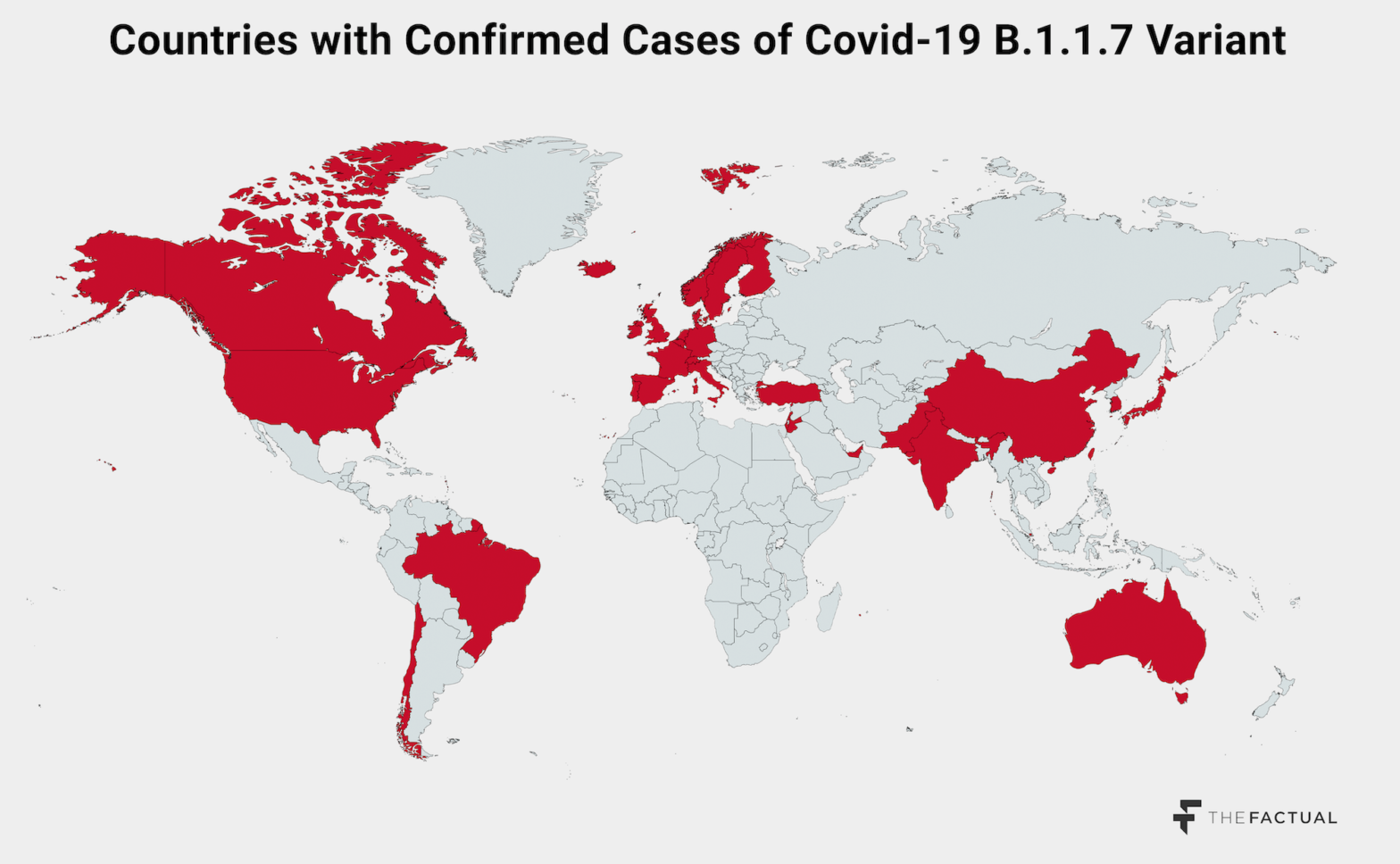
In a cruel twist, 2020 left parting gifts: at least two new, seemingly more dangerous variants of Covid-19. B.1.1.7 was first identified in the UK in September and has recently accounted for more than half of new cases in the country. B.1.351 is the variant behind a new surge in cases in South Africa. Both show signs of being significantly more transmissible than non-variant Covid-19, and B.1.1.7 has already been identified in dozens of countries around the world, including the U.S. While scientists are relatively certain neither is more deadly, higher transmissibility could spell big trouble.
This week, The Factual looked at 24 articles from 21 sources to clarify just how potentially dangerous these new Covid variants are.

Please check your email for instructions to ensure that the newsletter arrives in your inbox tomorrow.
What We Think We Know
The importance of clarity and consistency in messaging was made clear early on in the pandemic, and many articles about these new variants seem to be forthright about the details of these new strains without engaging in fear-mongering or clickbait headlines. Here’s what we know reasonably well.
Transmissibility: Both strains seem to demonstrate a greater level of transmissibility, meaning they spread easier from person to person. While the science is still being checked and triple-checked, the B.1.1.7 variant seems to be as much as 70% more transmissible than the non-variant Covid-19. Less is known about B.1.351, but it seems at least as dangerous as B.1.1.7.
This increased transmissibility is a result of the routine genetic mutation that viruses (and, indeed, all lifeforms) undergo during replication or reproduction. For both strains, mutations to the spike protein — the protein that allows the virus to attach to uninfected cells — seem to make the virus better at infecting human cells. Additionally, early evidence also seems to suggest that the new variants result in higher viral loads, meaning infected individuals are carrying more of the virus.
Source: The Conversation
Deadliness: A clear further risk with new mutations of a virus is that they could become more deadly for those who are infected. Thankfully, for these new Covid-19 variants the increase in transmissibility does not appear to be accompanied by an increase in the severity of the disease.
However, the virus itself doesn’t need to cause more severe effects to still result in an increase in deaths. For example, if the virus is much more transmissible, that can result in an exponential rise in cases and an inability to provide life-saving care to the cases that are severe. With hospitals around the U.S. already reaching maximum capacity, and non-Covid patients being turned away, an exponential increase in cases could very well lead to more Covid-related and non-Covid-related deaths.
Mitigation: Scientists are very clear that the nature of the threat from the virus has not fundamentally changed in terms of how the virus spreads and what we can do to stop its spread. The virus is still a respiratory illness that spreads through the air and close contact with other people. This means that the mitigation strategies already in place still apply and, if anything, are more important than ever.
Countries are responding by enacting more stringent applications of measures that were largely already in place. In London and the southeastern UK, where B.1.1.7 really came to the fore, a stringent lockdown has been enacted to halt the spread of the virus, reversing a decision to loosen restrictions for the holidays. South Africa has enacted strong measures as well, including banning public gatherings and the sale of alcohol and making mask wearing in public mandatory. Abroad, many countries have halted flights from the UK and South Africa, reflecting that the danger for contagion is just too great.
Testing: A plausible risk is that the virus might mutate in such a way that leads positive cases to avoid identification, thereby necessitating new tests. Luckily, the mutations that the virus underwent did not interfere with our ability to identify positive cases with current testing technology. Though, for example, the virus did modify the spike protein that current tests look for—also known as the S gene—tests look for a number of signals, not just one. Scientists are now working to estimate the prevalence of B.1.1.7 based on the number of positive tests without the S gene, cases known as S-gene dropouts.
Vaccines: Perhaps the biggest question on everyone’s minds is whether the stream of newly-approved vaccines will retain effecitveness against these new variants. While testing is still underway, there is no evidence to suggest that the vaccines will see any significant change in efficacy. Mutations are typically subtle and are unlikely to drastically alter the biology of the virus in a short period of time, and the vaccines are designed to attack the virus from several angles, meaning that the “broad immune response…that targets several areas of the spike protein” will continue to work.
Please check your email for instructions to ensure that the newsletter arrives in your inbox tomorrow.
The Big “Ifs”
Much of what we know about the variants, beyond the likely increase in transmissibility, is none too alarming on the surface. However, there are some factors that we aren’t totally sure of just yet that could create big problems.
Spread: These new variants show yet another way pandemic response has fallen short. Understanding the genetic variations in the virus requires routine genetic sequencing to identify new strains, but very few countries have been investing the resources to do so. While the UK invested early on to sequence cases to track the genetic variations, a CDC strain surveillance team in the U.S. was set up only in November, and the CDC had only sequenced 51,000 samples by the end of 2020, out of nearly 20 million cases. This not only means that we have no idea how widespread the B.1.1.7 variant is in the U.S., it means that we may have our own distinct variants without even knowing.
From the paltry amount of genetic sequencing that we do undertake in the U.S., we know for sure that B.1.1.7 is in California, Florida, and Colorado, but the circumstances of those cases is worrying. All three instances involve no significant travel history, meaning that the variant is already in the U.S. and spreading via community transmission. The optimistic interpretation of this is that there may be a few, isolated pockets of this variant in the U.S. The pessimistic view, however, is that the U.S. is on the cusp, and well past the point of return, of a fast-moving outbreak that will dwarf what we’ve seen so far, absent strong response measures. The UK saw the B.1.1.7 variant appear in September but account for more than 60% of cases in London just months later, accompanied by the worst outbreak yet. The same could be underway in the U.S.
Susceptibility: One of the reprieves of Covid-19 has been that children are relatively less susceptible to infection. This has enabled some schooling to proceed under modified protocols, even while workplaces have been shut and public gatherings disbanded. However, the emergence of the new variants has corresponded with increases in rates of infection and severe cases among children and young adults. While some of this can likely be explained by schools remaining open and young people being likely to disregard social distancing guidance, for example, this doesn’t seem to be the whole story. Scientific testing continues, but many worry that the B.1.1.7 variant can actually more easily infect young people than non-variant Covid-19, which may mean some previously effective Covid mitigation strategies will need to be reconsidered.
Exponential Risk: Some have pointed out that a significantly more transmissible virus is actually much more worrisome than a virus that just leads to more severe cases. In the latter instance, the virus still only affects the same number of people, though it kills more of them, but with the former, many, many times more people may become infected—and potentially die.
“Kucharski compares a 50 percent increase in virus lethality to a 50 percent increase in virus transmissibility. Take a virus reproduction rate of about 1.1 and an infection fatality risk of 0.8 percent and imagine 10,000 active infections—a plausible scenario for many European cities, as Kucharski notes. As things stand, with those numbers, we’d expect 129 deaths in a month. If the fatality rate increased by 50 percent, that would lead to 193 deaths. In contrast, a 50 percent increase in transmissibility would lead to a whopping 978 deaths in just one month—assuming, in both scenarios, a six-day infection-generation time.” – Zeynep Tufekci, The Atlantic
But the risks don’t end there. The problem with an exponential increase in the number of cases, and indeed with the idea of letting the virus run its course through a population in the hopes of achieving herd immunity, is that this creates that many new opportunities for the virus to mutate further. This could lead to further changes in transmissibility, new variants that allow for reinfection, a more deadly combination of both transmissibility and severity, or even variants that, at some point, entirely undermine our vaccine efforts.
Any such change could have big positive or negative ramifications for the trajectory of the virus. Epidemics like H1N1 and various strains of Ebola proved to be too deadly to be truly disastrous on a global scale: they tended to kill their carriers at a rate that limits the ability of the virus to spread to new hosts. But those viruses may have been just a mutation away from a much more dangerous, if less lethal, form. Covid-19 may also be just a few mutations away from such a seismic shift, for better or for worse. Such mutations are a “once-in-a-million event,” but “but one-in-a-million events may become a lot more common when you have a million new cases every four days, as the U.S. now does.”
Appendix
This appendix shows each of the articles used to inform the findings of this article, as well as how the articles scored according to The Factual’s credibility algorithm. To learn more, read our How It Works page.